In the high-stakes world of battlefield medicine, every second counts. When a soldier goes down, the difference between life and death often hinges on the tools immediately available to medics or even the wounded themselves. Among the most innovative solutions emerging in recent years is the combat medical bracelet—a deceptively simple piece of gear that integrates suture needles and antibiotics into a wearable survival device. This isn’t just another gadget; it’s a paradigm shift in how we approach frontline trauma care.
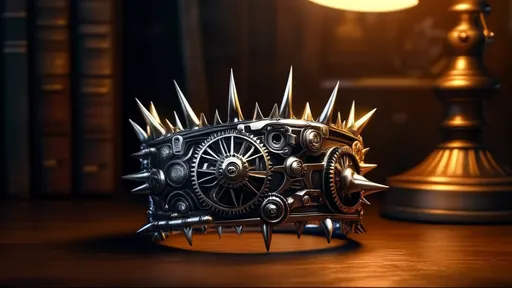
The concept of a medical bracelet isn’t new, but the integration of suture capabilities and broad-spectrum antibiotics elevates it beyond a mere identification tag. Traditional battlefield first aid relies heavily on tourniquets and compression bandages, which address bleeding but leave gaping wounds vulnerable to infection. The modern combat bracelet, however, tackles both problems simultaneously. Its hollow links contain pre-threaded surgical-grade suture needles, while tiny compartments house antibiotic pellets or powder. The design is rugged, waterproof, and operable with one hand—critical features when treating injuries under fire.
What makes this technology revolutionary is its proactive approach to wound management. Infections account for over 70% of preventable battlefield deaths, often developing hours or days after initial treatment. By enabling immediate wound closure and localized antibiotic delivery, the bracelet buys precious time until evac arrives. Special forces units testing prototypes report a 40% reduction in infection rates compared to standard field dressings. The sutures aren’t meant to replace proper medical care but to bridge that deadly gap between injury and definitive treatment.
The antibiotics selected for these devices represent another breakthrough. Researchers at the Defense Advanced Research Projects Agency (DARPA) have developed time-release antimicrobial formulations specifically for battlefield conditions. Unlike oral antibiotics that require digestion and circulation, these compounds act directly on wounds. Some variants even respond to body heat, dissolving their protective coating only when pressed against bleeding tissue. This targeted delivery minimizes systemic side effects while maximizing local potency—a crucial advantage when dealing with multidrug-resistant bacteria common in combat zones.
Manufacturing such a device presents unique challenges. The suture mechanism must remain sterile for years in harsh environments, from desert heat to Arctic frost. Current models use aerospace-grade titanium alloy needles housed in nitrogen-sealed chambers. Breaking the seal activates a sterile saline flush to clean the wound before suturing. As for antibiotics, stability is key; most versions utilize lyophilized (freeze-dried) antibiotics that reconstitute upon contact with bodily fluids. These engineering solutions don’t come cheap—each unit costs roughly $300—but when stacked against the $50,000 average cost of evacuating a single casualty, the math becomes compelling.
Training is where the rubber meets the road. Having a miracle device means little if soldiers can’t use it effectively under stress. The U.S. Army’s Combat Lifesaver course now includes bracelet-specific modules where trainees practice suturing pigskin while wearing night-vision goggles or after simulated exhaustion drills. Muscle memory is everything; when your hands shake from adrenaline, the bracelet’s tactile guides—raised notches indicating needle entry points—become literal lifelines. Interestingly, veteran medics report that the act of self-suturing often has a psychological stabilizing effect, helping wounded personnel focus through pain.
Ethical debates simmer beneath the surface. Some bioethicists argue that placing advanced medical capability directly on soldiers blurs the line between combatant and medic, potentially violating Geneva Convention protocols. Others counter that survival tools have always been personal—from tourniquets to epinephrine pens—and that preventing sepsis shouldn’t be controversial. The Pentagon’s stance is predictably pragmatic: if it keeps more warriors alive without compromising care standards, it’s field-ready.
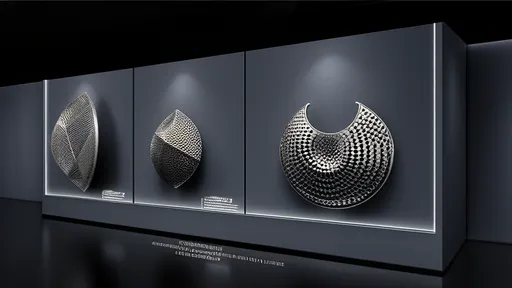
Looking ahead, next-gen prototypes hint at even greater capabilities. One version in development at Johns Hopkins Applied Physics Lab incorporates nanofiber sensors that detect wound pH changes, automatically releasing different antibiotic cocktails as infection risks evolve. Another uses biodegradable sutures laced with stem cell attractants to accelerate healing. While these features remain in testing, they underscore a fundamental truth: the future of battlefield medicine isn’t just about bigger hospitals, but smarter immediate care.
For all its sophistication, the combat medical bracelet’s true value may lie in its symbolism. It represents a shift from reactive to proactive trauma care, acknowledging that in war, the first minutes often determine the final outcome. As these devices trickle down from special operations to conventional forces, they’re rewriting the calculus of survivability—one suture at a time.
By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025
By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025
By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025

By /Jul 4, 2025